Burnout among healthcare workers isn’t new—awareness of the problem was rising long before COVID-19. The pandemic, however, cast a harsh light on the implications of the issue—for workers, for employers, and ultimately, for patients.
Healthcare employee burnout has taken on new urgency. After seeing physicians, nurses, and other healthcare workers buckle under the intense weight of caregiving during the pandemic, healthcare organizations across the country have introduced new policies and procedures designed to head off burnout.
Our survey of 321 industry professionals¹ found that healthcare organizations made the following changes during the pandemic:
- 39% provided more flexibility in work schedules
- 36% added support for mental health
- 29% introduced new vacation and sick leave policies
- 24% expanded learning and development opportunities
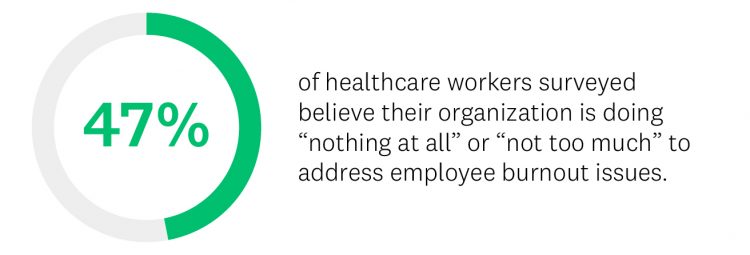
Yet despite these changes, healthcare workers remain stressed. Turnover is up at many hospitals and healthcare systems—the result of nurses and physicians at the brink—and many in the industry feel their employers aren’t doing enough to help with the problem. When asked how much their organization is doing to address employee burnout, 1 in 4 healthcare workers we surveyed said “not too much,” while another 1 in 4 said “nothing at all.”
Creating policies to address healthcare worker burnout is a start, but these changes clearly aren’t enough. How do you know if your policies are effective? Efficient data collection along the way can help refine a program so it’s as effective as possible over the long run. Here’s what to consider.
Identifying healthcare worker burnout
For healthcare workers, burnout can be driven by a variety of factors: staffing issues, unforgiving schedules, taxing work environments, and tedious insurance-mandated record-keeping. Those factors may lead to a combination of severe emotional stress and depersonalization (feeling dehumanized by the work), and low sense of professional efficacy, said Douglas A. Mata, MD, MPH, a pathologist and public-health researcher. The relentless pressure introduced by COVID-19 exacerbated the problem, but it’s far from the only source.
Well before the pandemic began, many healthcare workers were already feeling stressed, exhausted, and defeated. A 2017 paper published by the National Academy of Medicine reported that over 50% of U.S. physicians were experiencing substantial symptoms of burnout, while up to 37% of nurses had a high degree of emotional exhaustion. The pandemic took those feelings to new heights: 89% of healthcare workers we surveyed said it has affected the mental health and wellbeing of their colleagues.
“Doctors who are unhappy are more likely to quit their job,” said Dr. Mata. That’s true for other healthcare workers, too: one report concluded that nearly 32% of nurses who quit their jobs in 2018 did so partly or entirely because of burnout. Given that screening, hiring, and onboarding a replacement can cost as much as 200% of an employee’s annual salary, employee turnover is more than just disruptive—it can also be incredibly costly.
In many cases, employees just want to know that they’re being heard.
Douglas A. Mata, MD, MPH, pathologist and public-health researcher
Long-term job burnout can have serious ramifications. For healthcare workers, these can range from a general distaste for going to work to clinical depression and even suicidal tendencies in the most extreme cases. And when doctors, nurses, and other healthcare workers feel spent, it can also affect those who employ them.
In addition to the issues surrounding provider wellbeing, there are also safety issues at stake. Disengaged healthcare workers might leave patients less satisfied with the care they receive, said Dr. Mata. “Some studies have suggested that burnout leads to decreased quality of care,” he explained.
Use feedback to improve employee wellbeing
Learn about our enterprise solutions to help you develop and retain a healthy and engaged workforce.
Collecting the right insights
Healthcare employers can’t take proactive steps to mitigate the problem unless they first know how their employees are feeling. Conducting a simple, straightforward survey to assess the wellbeing of workers can be beneficial, said Dr. Mata. “In many cases, employees just want to know that they’re being heard.”
With more information about current levels of job burnout and the driving factors, employers can then make specific changes that promote a healthier, happier work environment. For instance, if numerous workers note that it’s difficult to find adequate childcare that fits their schedule, hospitals and large healthcare systems might consider adding on-site day care. If many doctors and nurses complain about being bogged down by paperwork and electronic record-keeping, hiring additional support staff to focus on such administrative tasks or investing in intelligent automation technology could free them up to focus on direct patient care.
For some healthcare organizations, simply changing policies around call schedules or tweaking sick and vacation leave policies might do the trick. Even just letting healthcare providers have more flexible work schedules—a benefit that 36% of healthcare workers we surveyed said they received in the wake of the pandemic—can have major benefits. According to Dr. Mata, “Everyone feels better if they have more control.”
Once employee wellness programs are launched, healthcare organizations can continue to use surveys to gauge their effectiveness. “The data you collect can help you refine your approaches and calculate the impact that different initiatives are having in your organization,” explained Sara Dowling, SurveyMonkey’s senior director of Learning and Development.
Overcoming employees’ fear of reporting burnout
One key challenge with tracking employee wellbeing is the stigma associated with reporting burnout. Given that some doctors may be hesitant to report mental health issues for fear of jeopardizing their licensing, employers will need to broach the issue with care. Letting employees know upfront that their survey responses are anonymous can help reduce concerns, enabling you to get more accurate, honest feedback from your employees.
When developing surveys, purposeful language can go a long way. Rather than positioning the survey as being about mental health or burnout, Dr. Mata suggested focusing healthcare worker assessments on wellbeing and engagement. “I’d liken it to professional fulfillment,” he said. By giving the topic a more positive spin, employers can obtain critical information without putting employees on the defense.
By tracking employee burnout, understanding what causes it, and developing empathetic, supportive programs focused on wellbeing, healthcare organizations can improve employee engagement—and by extension, transform patient outcomes and experiences.
To learn more and discover tips for writing healthcare surveys that drive results, check out our in-depth guide to healthcare surveys.
¹SurveyMonkey research of 321 U.S.-based healthcare professionals conducted in May 2021, using SurveyMonkey Audience.